Surprisingly it wasn’t that long ago when American surgeons played the important mid-wife role to the concept of offering clear protocols for managing major trauma that allowed doctors to deal with complicated clinical situations in a controlled and structured way. Advanced Trauma Life Support (ATLS) is now regarded as the common international language of trauma care and the course has trained over 700,000 doctors worldwide in over 50 countries.
My ATLS certification was going to run out later this year and I was fortunate enough to secure a place on a course in Edinburgh when a candidate dropped out at the last minute. I remember the time when a two-year despairing waiting list was the norm for what was then not even a requirement for surgical trainees but I had the foresight to know the impact and importance it was going to make and had always got myself certified.
Thanks to the internet, I was able to rapidly assess what upcoming courses were available and I made my intentions (erm, enthusiasm) clear via a mass e-mail campaign (heh). The fact that I stressed I could pay pronto and was available immediately put me at a distinct advantage – availability in cash and person always got the desired attention.
The setting was the Lister and the usual mixed bunch of ATLS provider candidates consisted of doctors from specialties ranging from General Practice, Intensive Care, Accident and Emergency, Acute Medicine, General Surgery, Orthopaedics and Trauma and Anaesthetics, and grades from FY2s/SHOs to Consultant level, with half a dozen nursing staff from the Royal Infirmary of Edinburgh as observers.
After the registration process of having our mug shots taken by digicam and candidates tentatively getting to know one another over bladder bursting cups of coffee and cold Saran wrapped sandwiches we had the welcoming talk given by our enthusiastic host followed by brief introductions from each member of the Faculty board. I forgot how it had always been de rigeur for each candidate to stand up in front of everyone and give an impromptu introduction of themselves, and (here is what I like) tell everyone something unique or interesting about themselves (mine: I almost made it to Everest Base Camp…..pfffffffffft) – which was a great way to break the ice in later social settings.
After the familiar important ATLS mantra of A, B, C, D and E (Airway maintenance with cervical spine immobilization; Breathing and ventilation; Circulation with haemorrhage control; Disability: Neurologic status; Exposure/Environmental control: Completely undress the patient, but prevent hypothermia) was drummed into us, the audiovisual lectures whizzed by in rapid succession. I found the more memorable talks had audience participation and simple audio-visual aids to reinforce key messages: to wit, three candidates having a race squirting into a bucket from a short, fat needle, long venflon and an even longer and thinner CVP line attached to syringes full of dihydrogen monoxide to illustrate Poiseuille’s law.

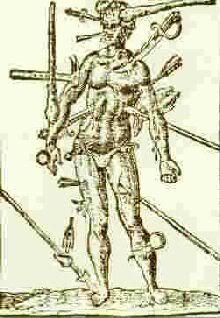
The enjoyable parts (beside the social) were when we as candidates got to DO things. The skill stations were fun as it allowed blood to circulate around our brains and hands instead of our sedentary feet and where techniques such as surgical cricothyroidotomy, endotracheal intubation, chest drains, CVP line insertions, log rolling and practice moulage got going. Reading about something is one thing…it’s only when you get to do something do you realise the nuances specific to practical procedures that you can’t glean from a page of text. It was imperative that everyone should have thoroughly read and highlighted to death the creased and spine destroyed bended manual before attending the course to get maximum benefit.
I noticed the more dramatic procedures of diagnostic peritoneal lavage and pericardiocentesis got relegated to a discussion level when these were actively taught as a procedural skill in the past. But I always thought the chances of an average ATLS provider getting to do these in real life to be unrealistic (I have done a pericadiocentesis only once on a cardiac arrest patient) as the availability and ease of skilled specialty help and imaging such as spiral CT and ultrasound scans in a hospital setting becomes more accessible.
Giovanni’s restaurant (oddly situated on the top floor of the Lister) was the setting for the social. Everyone was friendly and easy going and stories and anecdotes were exchanged over glasses of wine and pork (absolutely perfect for me *rolls eyes*). It was unsurprising that topics such as the recent MTAS debacle and mini-exodus of doctors to other Anglo-phone countries had to rear its gorgeous head.
Oh, the last day with the written exam and moulage was…GREAT FUN!! To coordinate and use all the principles one had (supposedly) learnt in a test situation was actually stressful on the spot. Having a clear, cool calm head, be able to think logically, be able to make sure that each part of the ABCs were effectively managed when identified, skilled help was called when needed, necessary investigations ordered and constant re-evaluations were done were all keys to not screwing up and unwittingly “kill” your patients.
I think such a course should be mandatory for all whose work deals with trauma patients (well, that is pretty near much all doctors then – at least when they start their careers) and should be introduced on a basic form at the undergraduate level. But there is always the question of time and funding…I was surprised that all the FY2s had to fund their own course when not too long ago study leave budgets at least offered a financial buffer. But such is the state of the beleaguered cash strapped NHS these days. Although at times the moulage scenarios were artificial and contrived, it was a necessary evil to force the candidates to think through the principles in order to see and apply them in action so that in real life, everyone will understand and be talking the same vocabulary when both assessment and resuscitation goes on simultaneously by a team in the resuscitation bay. I like the beautiful logic inherent in the system of patient assessment and management.
Thanks has to be extended to the administrative and catering staff and to all the volunteers who gamely got themselves into make-up mode of wounds, cervical collars and splints, and role-playing combative or near moribund patients as the situation demanded in the moulage. And finally extra thanks has to be extended to all the accommodating, enthusiastic and good-humoured faculty staff for taking time from their busy clinical schedules to teach another rag-tag bunch of plebeians to make the world a safer place.
Oh, the last day with the written exam and moulage was…GREAT FUN!! To coordinate and use all the principles one had (supposedly) learnt in a test situation was actually stressful on the spot. Having a clear, cool calm head, be able to think logically, be able to make sure that each part of the ABCs were effectively managed when identified, skilled help was called when needed, necessary investigations ordered and constant re-evaluations were done were all keys to not screwing up and unwittingly “kill” your patients.
I think such a course should be mandatory for all whose work deals with trauma patients (well, that is pretty near much all doctors then – at least when they start their careers) and should be introduced on a basic form at the undergraduate level. But there is always the question of time and funding…I was surprised that all the FY2s had to fund their own course when not too long ago study leave budgets at least offered a financial buffer. But such is the state of the beleaguered cash strapped NHS these days. Although at times the moulage scenarios were artificial and contrived, it was a necessary evil to force the candidates to think through the principles in order to see and apply them in action so that in real life, everyone will understand and be talking the same vocabulary when both assessment and resuscitation goes on simultaneously by a team in the resuscitation bay. I like the beautiful logic inherent in the system of patient assessment and management.
Thanks has to be extended to the administrative and catering staff and to all the volunteers who gamely got themselves into make-up mode of wounds, cervical collars and splints, and role-playing combative or near moribund patients as the situation demanded in the moulage. And finally extra thanks has to be extended to all the accommodating, enthusiastic and good-humoured faculty staff for taking time from their busy clinical schedules to teach another rag-tag bunch of plebeians to make the world a safer place.


2 comments:
Hi, guantanamera121212
не факт
Post a Comment